Interview with Columbia University Public Health Students
For tonight’s Grand Rounds at Columbia University, I did an interview with FPOP (Food Policy and Obesity Prevention).

Food Policy Expert Marion Nestle on the Heinz-Kraft Deal, GMOs, and the Secret Ingredients to Healthy School Lunches
March 31, 2014—Years before the Reagan Administration decreed that ketchup was a vegetable, Marion Nestle saw the connections between the dinner table and politics. Nestle, the nation’s leading advocate for good nutrition, will address the Mailman School in a Grand Rounds talk tomorrow and kick-off Public Health Fights Obesity, a month-long series of lectures and special events, including an April 16 symposium on preventing childhood obesity.
Nestle, a professor and founder of the department of Nutrition, Food Studies, and Public Health at New York University, is the author of acclaimed books, includingFood Politics: How the Food Industry Influences Nutrition and Health, and most recently, Why Calories Count: From Science to Politics.
In anticipation of her Grand Rounds talk, the student group Food Policy and Obesity Prevention interviewed Nestle about everything from attempts to regulate Big Soda, GMO labeling, to school lunches done right.
The federal Dietary Guideline Advisory Committee recently published recommendations that for the first time considered issues of food sustainability. There has been a lot of controversy.
The guidelines have always been controversial, but never anything like this. I think this is an example of how worried the food industry is about the pushback about diet and health in America. Sustainability is the “S word” in Washington. The guidelines committee is trying to do is what I’ve been advocating for a very long time, which is to bring agricultural policy in line with health policy. Right now the policies are completely divorced.
At the same time you have Heinz and Kraft joining forces.
The food industry is in a defensive position because food and health advocates have been enormously successful in changing the market and changing people’s views. The fastest growing segment of the food industry is organics. The makers of processed foods are in retreat. Warren Buffett must think there’s plenty of money to be made in selling junk foods. I hope he’s wrong.
Is Big Food increasingly eyeing opportunities overseas?
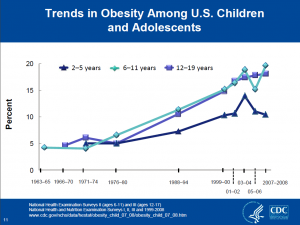
If you can’t sell it here, you sell it there. The best example of this is the soda industry, which is the subject of my next book. There has been a 10- to 15-year decline in sales of carbonated sweetened beverages in the United States. It’s one of the great successes of health advocacy. To compensate, Coke and Pepsi are increasingly focusing their efforts overseas. Expect obesity and its consequences to follow.
Speaking of global commerce, should we be concerned about trade agreements like the Transpacific Partnership?
Food and Water Watch called it “NAFTA on steroids.” It’s very hard to know what’s going on because the negotiations are being done in secret. People are worried that a lot of the protections we have against bad things in food will be taken away on the basis of violations of trade agreements.

Poster supporting a soda tax in Berkeley
Closer to home, here in New York we’ve heard a lot about attempts to legislate on soda with failed attempt to limit portion sizes. Other areas have had more luck—
Not luck—skill! The only place in the United States where a soda tax has been successful is Berkeley. They did everything about advocacy right. Instead of framing it as a health argument, they framed it as an argument against corporate power: Berkeley versus Big Soda. And there was an enormous grassroots effort to engage the entire community. Community organizing is classic public health. Nobody does it very often. But when it’s done, it works!
Another issue people have been talking about is GMO labeling.
I was on the FDA food advisory committee in 1994 when they were in the process of approving GMOs. Those of us who were consumer representatives told the FDA that it had to require labeling. I’m surprised it’s taken this long for there to be a major national uproar. From the beginning, the question was: if they don’t want labels, what are companies like Monsanto trying to hide?
Speaking of Monsanto, there was news this week that a chemical in their Round Up herbicide is a likely a carcinogen.
RoundUp also induces weed resistance, which has become an enormous problem for the industry. And most of it is used on GMOs. It’s a plant poison! Why would anyone think it would be good for health?
Are GMOs always bad?
The papaya that’s engineered to resist ring spot seems like a reasonable use of biotechnology to me. It saved the Hawaiian papaya industry. That’s the only example I can think of that’s beneficial. Most of the technology has been applied to commodity crops.
What about food insecurity? Can GMOs help?
If you want to help food-insecure nations, you need to empower them to do their own agriculture. That agriculture needs to be sustainable. GMO crops are not sustainable. They require seeds, fertilizer, and pesticides, every year.

President Obama signs the Healthy Hunger-Free Kids Act in 2010
According to a new Rudd Center study, more kids are eating fruit at school. At the same time, there’s a lot of pushback against healthy foods at school.
In 2010, Congress passed the Healthy Hunger-Free Kids Act. That was bipartisan. Today, bipartisan seems out of the question. The Republicans want to roll the Act back. There’s no question it’s working in most schools that have people committed to it. There are huge advances being made in school food that carry over to food outside school. Kids come home and they want different foods because they see that eating healthy foods is valued.
How much is this change tied to school leaders compared to funding?
More funding would help. But some of the poorest schools have cafeterias where you walk in and the food smells good. They’re making it happen by cooking onsite with USDA commodity foods, which are unprocessed and cheap. Someone who knows how to cook can turn USDA surpluses into good meals. But not every school does that. I’ve been in schools where the food was terrible, the kids weren’t eating it, and the plate-waste was astronomical. If the food service workers know the names of the kids, it’s a good sign the food will be good too.
For students interested in food and health, what sectors offer the most opportunity? Government? Nonprofit?
It depends on what you like. We need good people in government. It’s really important to have public health professionals work from within to make agencies like the FDA and Department of Agriculture do useful work. Everybody loves NGOs. It doesn’t matter which. Just do it!
Attend Marion Nestle’s Grand Rounds talk on April 1, 4:00-5:30 p.m., at Alumni Auditorium, 650 West 168th Street, or watch it on LiveStream.