Weekend Reading: Soda Science
Susan Greenhalgh. Soda Science: Making the World Safe for Coca-Cola. University of Chicago Press, 2024.
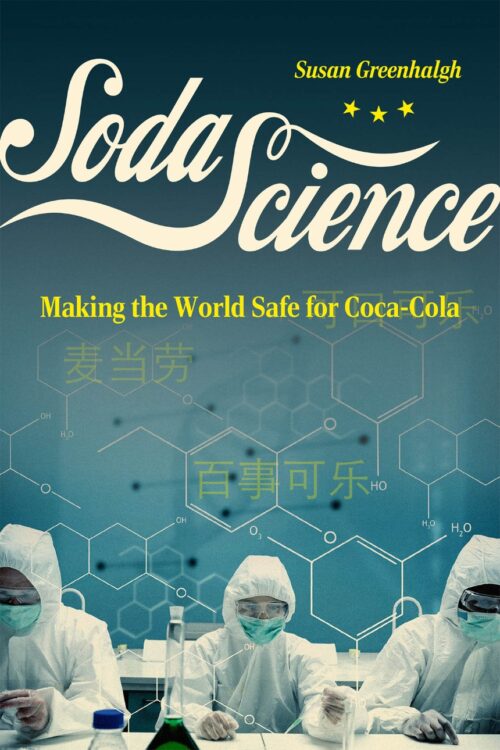
This terrific book picks up where I left off with Soda Politics: Taking on Big Soda (and Winning) (2015) and Unsavory Truth: How the Food Industry Skews the Science of What We Eat (2018).
Susan Greenhalgh’s focus, however, is on ILSI, the International Life Sciences Institute (now renamed the Institute for the Advancement of Food and Nutrition Sciences). ILSI is a classic industry front group, It was created originally by Coca-Cola to make sure science promoted corporate interests. It is funded by big food companies. It positions itself as an independent think tank. Hence: front group.
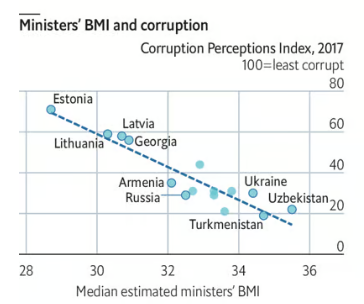
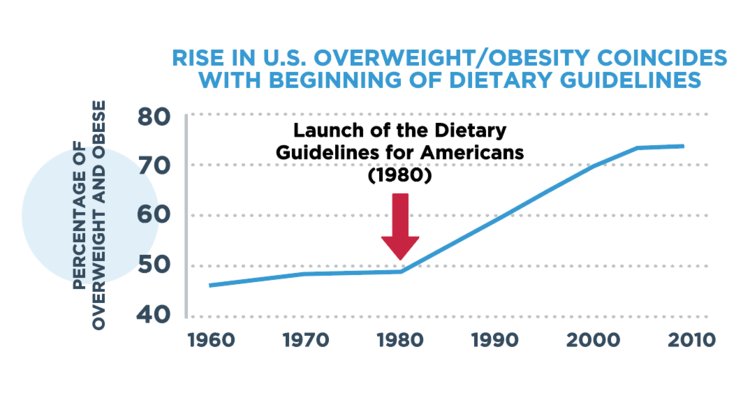
Soda Science documents how ILSI, working through personal connections (guanxi) at the Chinese Ministry of Health, convinced the Chinese government to target obesity prevention measures at physical activity (“move more”), rather than diet (“eat less,” or “eat better”).
The first half of the book tells the story of ILSI’s role in the Global Energy Balance Network, a group outed as funded by Coca-Cola (I wrote about this in 2015, particularly here, here, and here in The Guardian).
The second half gives an intimate, first-hand account of how science politics works in China.
Greenhalgh is a distinguished anthropologist. She retired from Harvard as as the John King and Wilma Cannon Fairbank Research Professor of Chinese Society (she is an expert on China). She uses social science methods—interviews and qualitative research as well as document review—to study this particular example of soda politics.
- The International Life Sciences Institute (ILSI): true colors revealed (October 3, 2019)
- ILSI tracked media responses to my book, Unsavory Truth (February 22, 2023)
The story she tells here is fascinating in its own right and a great read.
It also makes one other point: social science methods are really useful in getting information unavailable any other way.
I say this because bench scientists tend to look down on qualitative research and consider it non-research. I disagree. I think qualitative research is essential, and has plenty to contribute. This book is a great example of why.