My latest publication: Preventing Obesity
JAMA Internal Medicine has just published an editorial I wrote: Preventing Obesity—It Is Time for Multiple Policy Strategies
As it explains, it is a commentary on a research article by Joshua Petimar, et al, Assessment of Calories Purchased After Calorie Labeling of Prepared Foods in a Large Supermarket Chain
Both papers are behind paywalls, but here are the key points of the supermarket article:
Question Was calorie labeling of prepared foods in supermarkets associated with changes in calories purchased from prepared foods and potential packaged substitutes?
Findings In this longitudinal study of 173 supermarkets followed from 2015 to 2017, calories purchased from prepared bakery items declined by 5.1% after labeling, and calories purchased from prepared deli items declined by 11.0% after labeling, adjusted for prelabeling trends and changes in control foods; no changes were observed among prepared entrées and sides. Calories purchased from similar packaged items did not increase after labeling.
Meaning Calorie labeling of prepared supermarket foods was associated with overall small declines in calorie content of prepared foods without substitution to similar packaged foods.
I was really interested in this study because the “large supermarket chain” that supplied reams of data was so obviously Hannaford, which has long been ahead of the curve in trying to encourage customers to make healthier food choices.
In 2005, Hannaford initiated a Guiding Stars program that ranked–and still ranks–products by giving them zero to three stars depending on what they contain.
I wrote about the first-year evaluation of this program way back in 2006. It did help customers to make better choices.
Now, all these years later, the FDA is contemplating doing some kind of front-of-package label. As I said, Hannaford is way ahead.
But the point of my editorial is that single interventions rarely do better than what this study found.
I argue here for trying multiple strategies at once:
My interpretation of the current status of obesity prevention research is that any single policy intervention is unlikely to show anything but small improvements.
Pessimists will say such interventions are futile and should no longer be attempted.
Optimist that I am, I disagree. We cannot expect single interventions to prevent population-basedweight gain ontheirown,but they might help some people—and might help even more people if combined simultaneously with other interventions.
….Widespread policy efforts to reduce intake of ultraprocessed foods through a combination of taxes, warning labels, marketing and portion-size restrictions, dietary guidelines, and media education campaigns, along with policies for subsidizing healthier foods and promoting greater physical activity, should be tried; they may produce meaningful effects.
Politically difficult? Of course. Politically impossible? I do not think so.
Unless we keep trying to intervene—and continue to examine the results of our attempts—we will be settling for the normalization of overweight and the personal and societal costs of its health consequences.
Here’s Ted Kyle’s commentary on my commentary on ConscienHealth.

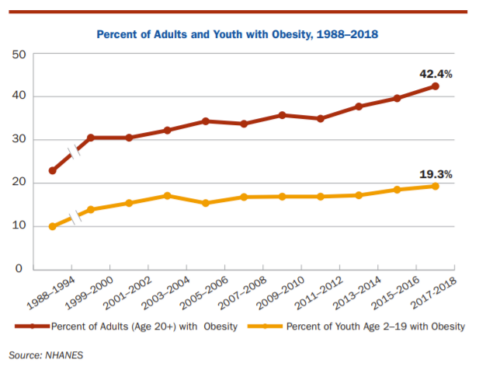



 This one was produced by the OECD (Organisation for Economic Co-operation and Development). It finds: “Almost one in four people in OECD countries is currently obese. This epidemic has far-reaching consequences for individuals, society and the economy. Using microsimulation modelling, this book analyses the burden of obesity and overweight in 52 countries (including OECD, European Union and G20 countries), showing how overweight reduces life expectancy, increases healthcare costs, decreases workers’ productivity and lowers GDP.”
This one was produced by the OECD (Organisation for Economic Co-operation and Development). It finds: “Almost one in four people in OECD countries is currently obese. This epidemic has far-reaching consequences for individuals, society and the economy. Using microsimulation modelling, this book analyses the burden of obesity and overweight in 52 countries (including OECD, European Union and G20 countries), showing how overweight reduces life expectancy, increases healthcare costs, decreases workers’ productivity and lowers GDP.”