The FDA Food Program’s “Deliverables” for chronic disease prevention: your personal responsibility
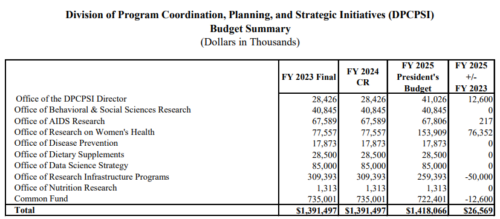
The FDA has announced its 2025 Priority Deliverables for the Human Food Program.
These cover the microbial and chemical safety of foods, but I am especially interested in what the FDA is and is not doing about nutrition and chronic disease prevention—something mentioned by FDA Commissioner Robert Califf as a priority for American public health.
Based on FDA’s Nutrition Initiatives, the deliverables begin with:
FDA’s Role in Empowering Consumers to Build Nutritious Diets that Support Health and Wellness
Using a risk management approach, we focus our efforts in FY 2025 on labeling and other initiatives to help consumers make more informed choices about the food they eat, and, for those who rely on certain critical foods, such as infant formula, as their sole source of nutrition, we work to make sure those products are safe, properly labeled, and nutritionally sound.
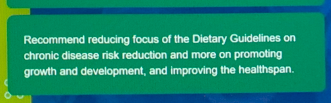
As for the Human Food Program’s priority policy initiatives:
- Update FDA’s Nutrient Content Claim “Healthy”
- Propose Front-of-Package Nutrition Labeling:
- Support Reductions in Sodium in the Food Supply
- Increase the Resiliency of the U.S Infant Formula Market
The deliverables do mention diet-related chronic disease in the contexts of sodium and research.
- We will also collaborate with our federal partners and engage with key stakeholders to enhance sodium-related data sharing and learnings, as part of these efforts to help reduce diet-related chronic diseases and deaths associated with high sodium intake, such as hypertension and stroke.
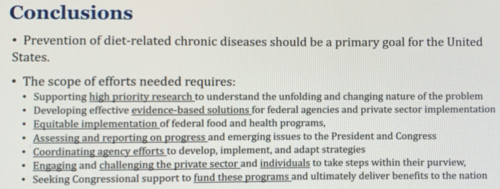
- We will continue to collaborate with other federal agencies on developing and advancing a nutrition research agenda, including accelerating high-quality research to better understand the mechanisms between ultra-processed foods and poor health outcomes.
Despite Commissioner Califf’s statements, it looks like the Human Food Program is not particularly interested in chronic disease prevention or policy approaches to improving the environment of food choice.
Instead, its policies put the burden of responsibility on you as an individual to make healthier choices—not to find ways to counter the food industry’s marketing imperatives.
The FDA’s Human Food Program is all about empowering consumers. Good luck with that.
Yes, the FDA is grossly underfunded and handicapped in what it can do, and yes, addressing environmental determinants of chronic disease would encounter opposition from vested interests.
But the FDA is an agency of the Public Health Service. It needs to do better.
The Human Food Program should be taking the lead in addressing Commissioner Califf’s stated concerns
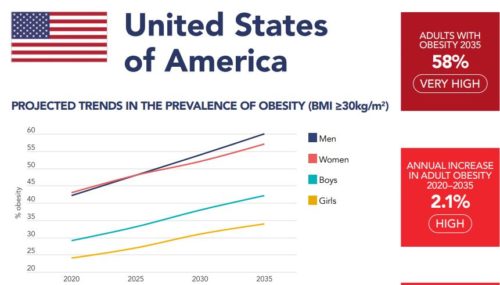
- The big issue is chronic disease, on which we are “doing terribly.”
- We have to deal with the marketing of ultra-processed foods designed to make you hungry for more.
These issues are consistent with the new administration’s Make America Healthy Again campaign. Let’s hope that works.