Looking ahead: food politics in 2012
My monthly Food Matters (first Sunday) column in the San Francisco Chronicle takes out a crystal ball…
Q: What’s on the food politics agenda for 2012? Can we expect anything good to happen?
A: By “good,” I assume you mean actions that make our food system safer and healthier for consumers, farmers, farm workers and the planet.
Ordinarily, I am optimistic about such things. This year? Not so much. The crystal ball is cloudy, but seems to suggest:
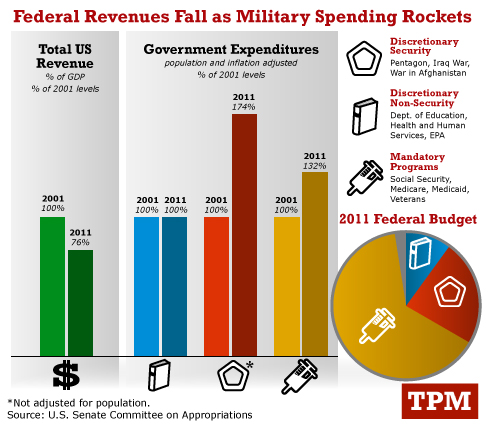
Political leaders will avoid or postpone taking action on food issues that threaten corporate interests. Sometimes Congress acts in favor of public health, but 2012 is an election year. Expect calls for corporate freedom to take precedence over those for responsible regulations. Maybe next year.
Something will happen on the farm bill, but what? Last fall’s secret draft bill included at least some support for producing and marketing fruits and vegetables, and only minimal cuts to SNAP (food stamps). Once that process failed, Congress must now adopt that draft, start over from scratch or postpone the whole mess until after the election.
SNAP participation will increase, but so will pressure to cut benefits. With the economy depressed, wages low and unemployment high, demands on SNAP keep rising. In 2011, SNAP benefits cost $72 billion, by far the largest farm bill expenditure and a tempting target for budget cutters. While some advocates will be struggling to keep the program’s benefits intact, others will try to transform SNAP so it promotes purchases of more healthful foods. Both groups should expect strong opposition.
Childhood obesity will be the flash point for fights about limits on food marketing. The Lancet recently summarized the state of the science on successful obesity interventions: taxes on unhealthy foods and beverages, restrictions on marketing such items, traffic-light front-of-package food labels, and programs to discourage consumption of sugar-sweetened drinks and television viewing. Expect the food industry to continue to get Congress to block such measures, as it did with U.S. Department of Agriculture school nutrition standards (hence: pizza counts as a vegetable).
The Federal Trade Commission will postpone release of nutrition standards for marketing to children. Although Congress asked for such standards in the first place – and the standards are entirely voluntary – it just inserted a section in the appropriations bill requiring a cost-benefit analysis before the FTC can release them. Why does the food industry care about voluntary restrictions? Because they might work (see previous prediction).
The Food and Drug Administration will delay issuing front-of-package labeling guidelines as long as it can. The FDA asked the Institute of Medicine for advice about such labels. The institute recommended labels listing only calories, saturated and trans fat, sodium and sugars – all nutrients to avoid. Although the institute did not mention traffic-light labels, it did recommend check marks or stars, which come close. The food industry much prefers its own method, Facts Up Front, which emphasizes “good-for-you” nutrients. It is already using this system. Will the FDA try to turn the institute recommendations into regulations? Maybe later.
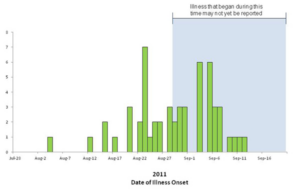
The FDA will (still) be playing catch-up on food safety. The FDA got through the 2011 appropriations process with an increase of about $50 million for its inspection needs. This is better than nothing but nowhere near what it needs to carry out its food safety mandates. The FDA currently inspects less than 2 percent of imported food shipments and 5 percent of domestic production facilities. The overwhelming nature of the task requires FDA to set priorities. Small producers think these priorities are misplaced. Is the FDA going after them because they are easier targets than industrial producers whose products have been responsible for some of the more deadly outbreaks? Time will tell.
On the bright side, the food movement will gather even more momentum. While the food industry digs in to fight public health regulations, the food movement will continue to attract support from those willing to promote a healthier and more sustainable food system. Watch for more young people going into farming (see Chronicle staff writer Amanda Gold’s Dec. 25 article) and more farmers’ markets, farm-to-school programs, school meal initiatives, and grassroots community efforts to implement food programs and legislate local reforms. There is plenty of hope for the future in local efforts to improve school meals, reduce childhood obesity, and make healthier food more available and affordable for all.
And on a personal note: In April, University of California Press will publish my co-authored book, “Why Calories Count: From Science to Politics.” I’m hoping it will inspire more thinking and action on how we can change our food system to one that is better for people and the planet.
Happy new year!