I’ve just turned in the copy-edited manuscript of Why Calories Count: From Science to Politics (pub date March 2012) and now have time to catch up on some questions:
Q. I was recently given to read a book titled “The China Study” which is based on research conducted in 1970’s in China by Dr. Colin Campbell. His main conclusion is that eating dairy and meat causes cancer. His resolution is that a plant-based diet (i.e. vegan) is the (only?) healthy diet for humans. This book has made strong enough of a point to convince several of my friends to “convert” to a vegan diet in order to save their health. Could you share some comments on the validity of the research and conclusions this book presents with regards to detrimental effects of dairy and meat on human health?
A. Campbell makes a forceful argument based on his interpretation of the research and on case studies of people whose diseases resolved when they became vegans. And yes I’ve seen Dr. Campbell’s new movie, Forks over Knives. The first half is a terrific introduction to how the current food environment promotes unhealthy eating. The second half promotes Dr. Campbell’s ideas about the hazards of meat and dairy foods.
Whether you agree with these ideas or not, the film is well done and worth a look.
Some scientists, however, interpret the research as demonstrating that people are healthier when they eat dairy foods. For example, the enormous consensus report on diet and cancer risk from the American Institute for Cancer Research and the World Cancer Research Fund concluded in 2007 that eating lots of red meat and processed meat is convincingly associated with an increased risk of colorectal cancer (but no others).
On the other hand, they found dairy foods to be associated with a decrease in the risk of colorectal cancer. They found limited and less convincing evidence that dairy foods might decrease the risk of bladder cancer but increase the risk of prostate cancer.
How to make sense of this? These are two food groups in the diets of people who consume many kinds of foods and who do many things that might increase or decrease cancer risk. Given this complexity, one food or food group seems unlikely to have that much influence on cancer when considered in the context of everything else people eat and do.
Nutrition research, as I am fond of saying, is difficult to do and requires interpretation. Intelligent people can interpret the studies differently depending on their point of view.
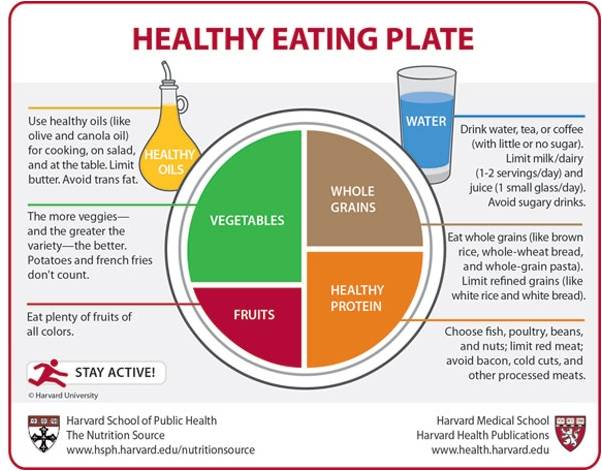
The new Dietary Guidelines say to cut down on saturated fats. Those are most plentiful in meat and dairy foods (plant foods have them, but in smaller amounts). Pretty much everyone agrees that plant-based diets promote health/ But whether they have to be 100% plant-based is highly debatable.
The new USDA MyPlate food guide suggests piling plant foods—fruit, vegetables, and grains—on 75% of your plate so the argument is really about what goes on the remaining 25%, what USDA calls the “Protein” section. You can put beans in that quarter if you don’t want to eat red meat, poultry, or fish.
Q. I’d love to hear your take on the recent walnut flap [accusations that the FDA now considers walnuts to be drugs]. I suspect walnuts got caught with such offenders as Pom, Froot Loops, and Juicy-Juice, but I’d love to find out what the FDA actually said about this. For some odd reason I don’t believe the article is presenting the whole truth.
A. This is a health claims issue. The FDA is not saying walnuts are drugs. It is saying that Diamond Walnut is claiming walnuts as drugs on package labels. How so?
The labels say the omega-3 fatty acids in walnuts may help lower cholesterol; protect against heart disease, stroke and some cancers (e.g. breast cancer); inhibit tumor growth; ease arthritis and other inflammatory diseases; and even fight depression and other mental illnesses. These are disease claims for which the FDA requires scientific substantiation.
The company’s petition did not provide that substantiation so the FDA issued a warning letter. In general, you should be skeptical any time you see a nutritional factor advertised for its ability to prevent or treat such a broad range of problems.
Q. A question about sugar and how it is counted: My books say: 4 g = 1 teaspoon = 15 calories. My Illy Caffe says 10 g of sugar, but 50 calories. Ingredients: coffee, sugar, potassium bicarbonate, potassium citrate. If the drink is 50 calories, shouldn’t it say 12 g or more for the sugar listing?
A. Sugar should be the only ingredient that has calories in this coffee but I’ve seen calorie lists that say 5 calories per gram for sugars. Food companies have some leeway in the way they compute calories. Illy may be using a method that gives 5 rather than 4. But the difference between 40 and 50 is hardly measurable and I wouldn’t worry about amounts this small, annoying as imprecise figures may seem.