Two articles I’ve written are in journals this week: a short one in Newsweek (!) and my monthly Food Matters column in the San Francisco Chronicle.
New York’s Calorie Counts: A Good National Model (Newsweek, April 30 online and May 10 in print)
The new health-care law contains an overlooked boost for nutritionists like me: by next year, all national chains with more than 20 locations must offer “clear and conspicuous” calorie information. It’s the most important obesity-related public policy since the USDA’s food pyramid. But reception to the new mandate has been muted so far, largely because the benefits of New York City’s similar 2008 law seem minor: one study found just 15 fewer calories were consumed per meal; another reported it was 30; and a third found that people ate more.
The problem with these studies is that they focus on Starbucks customers and fast-food goers in low-income neighborhoods—patrons who often care about convenience and value above all. They also fail to capture the long-term benefits of calorie counting, namely education and social pressure. Labels will offer case-by-case lessons in exactly what 1,000 calories looks like, and they may even spur restaurants to ease up on sugar and fat. (Denny’s, McDonald’s, and Cosi, among others, have debuted lighter fare in New York City.) Of course, much depends on the definition of “clear and conspicuous.” Still, the country’s nutritional literacy is about to improve—making my job a lot easier.
Sugary school meals hit lobbyists’ sweet spot (San Francisco Chronicle, Sunday, May 2)
Nutrition and public policy expert Marion Nestle answers readers’ questions in this monthly column written exclusively for The Chronicle. E-mail your questions to food@sfchronicle.com, with “Marion Nestle” in the subject line.
Q: I’m stunned by the amount of sugar my daughter is served routinely in school: candied cereals, flavored milk, Pop Tarts, breakfast cookies, fruit juice – 15 teaspoons of sugar, just in breakfast. Why no standards for regulating sugar in school meals, especially when obesity and diabetes are such concerns?
A: Politics, of course. The U.S. Department of Agriculture spends $12 billion a year on school meals. Kids buy foods from snack carts and vending machines. Food companies fight fiercely to protect their shares in that bounty.
If you watched “Jamie Oliver’s Food Revolution,” you witnessed the struggle to get sugary foods out of schools. Fifteen teaspoons – 60 grams and 240 calories – is a lot for breakfast, but kids get even more sugar from snacks, treats from teachers and birthday cupcakes.
Sugars were never a problem when we supported school lunch programs decently. That changed when schools ran out of money, sought vending contracts with soft drink companies and encouraged kids to buy sodas and snacks. Schools evaded restrictions on snack sales during lunch periods. Nobody paid much attention to what kids ate in schools – until kids began getting fatter.
Why no standards? Nobody wants to take on the sugar lobbyists.
In 1977, a Senate committee recommended an upper limit of 10 percent of calories from added sugars. This was so controversial that from 1980 to 2000, the Dietary Guidelines gave no percentages when they said “eat less sugar.” The 1992 food pyramid said “Use sugars only in moderation.” It defined moderation in teaspoons – for example, 12 a day in a diet of 2,200 calories, which comes to less than 10 percent of calories. By then, health officials in at least 30 countries had adopted the 10 percent sugar guideline.
A committee of the Institute of Medicine undermined that consensus. Because science provides only circumstantial evidence for the effects of sugars on obesity and other health problems, the committee suggested a safe maximum of 25 percent of calories. Sugar trade associations happily interpreted this percentage as a recommendation.
In 2003, the World Health Organization issued a research report restating the 10 percent guideline. Using the IOM report as evidence, sugar trade associations enlisted senators from sugar-growing states to lobby U.S. government officials to withdraw funding from WHO. They also lobbied governments of sugar-growing countries to oppose the 10 percent guideline. WHO dropped the 10 percent sugar guideline.
Dietary guidelines are the basis of federal nutrition policy. The 2005 guidelines advised limits on sugars without stating a percentage. In a footnote, the guidelines said that sugars could be part of a day’s “discretionary calories,” defined as 2 to 8 teaspoons a day. This is less than 10 percent of calories, but the guidelines do not say so explicitly.
Neither does the USDA’s 2005 pyramid, which personalizes diet plans based on age, activity level and gender. I, for example, am allowed 195 discretionary calories for added fats and sugars. If I use them all for sugars, I get to eat 12 teaspoons – about 10 percent of my daily calories. This is less than the amount your daughter ate for breakfast or the sugars in a 20-ounce soda. Hence: lobbying.
Will we get an explicit sugar policy when Congress gets around to reauthorizing the Child Nutrition Act? The draft bill says nothing about sugars but does require school foods to adhere to “science-based” nutrition standards based on the dietary guidelines. If so, this means a maximum of 10 percent of calories from added sugars.
The IOM has just released a “School Meals” report. This says that with careful planning, 10 percent should provide enough sugar discretionary calories to permit sweetened low-fat milk, yogurt and breakfast cereals. The IOM warns that without these sweetened foods, student participation rates and nutrient intakes might decline.
Sorry, but I don’t buy the “kids won’t eat it” argument. I’ve seen plenty of schools where kids eat unsweetened foods. Somehow, they survive. Kids will eat healthier foods when meals are prepared by adults who care what kids eat, as Oliver has demonstrated.
As for legislation, California led the way with the 2007 school food nutrition standards bill, which regulated soda sales and the amount of sugar in snacks. Companies responded by reducing the sugars in their products. Passing the Child Nutrition Act will help, but its big drawback is funding. The draft bill increases school reimbursements by only about 6 cents per meal, not enough to meet costs in many school districts and much less than the $1 increase that many believe necessary.
But with luck, 2010 will bring us national legislation and improved editions of the dietary guidelines and pyramid. Let’s hope these make it easier for schools to help kids cut down on sugars.
Note: Nestle and Malden Nesheim will speak about their new book, “Feed Your Pet Right,” at 3 p.m. May 22 at Omnivore Books in San Francisco and at 3 p.m. May 23 at Point Reyes Books in Point Reyes Station. Addition: Holistic Hound, Berkeley, Tuesday, May 18, 6:30 p.m.
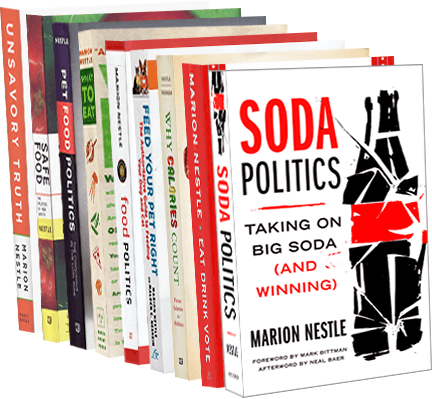
Marion Nestle is the author of “Food Politics,” “Safe Food” and “What to Eat,” and is a professor in the nutrition, food studies and public health department at New York University. E-mail her at food@sfchronicle.com and read her previous columns at sfgate.com/food. This article appeared on page K – 8.