Let’s Move Campaign gives up on healthy diets for kids?
In what Obama Foodorama calls “a fundamental shift in the Let’s Move campaign” Michelle Obama announced in a speech last week that she will now focus on getting kids to be more active.
Apparently, she has given up on encouraging food companies to make healthier products and stop marketing junk foods to kids.
This shift is troubling. Here’s why:
1. The shift is based on faulty biology.
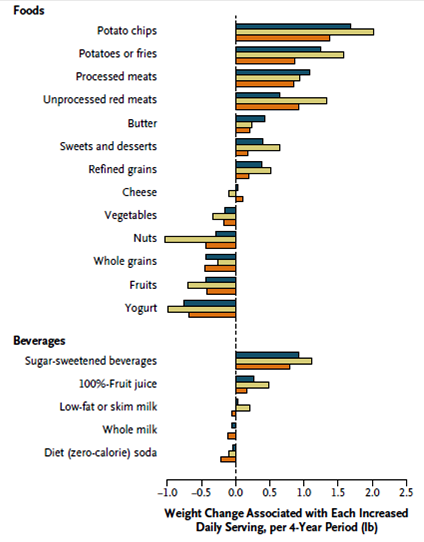
To lose weight, most people have to eat less whether or not they move more. For example, it takes about three miles of walking to compensate for the calories in one 20-ounce soda.
Activity is important for health, but to lose or maintain weight, kids also need to eat less. Sometimes they need to eat much less. And discouraging them from drinking sugary sodas is a good first step in controlling body weight.
But eating and drinking less are very bad for business. Food companies do all they can to oppose this advice.
2. It undercuts healthy eating messages.
On the one hand, Mrs. Obama says that she disagrees with this assumption: “kids don’t like healthy food, so why should we bother trying to feed it to them.”
But her speech implies that kids won’t eat healthfully unless forced to:
I want to emphasize that last point — the importance of really promoting physical activity to our kids…This isn’t forcing them to eat their vegetables. (Laughter.) It’s getting them to go out there and have fun.
3. It declares victory, prematurely.
Mrs. Obama says:
Major food manufacturers are cutting sugar, salt and fat from their products. Restaurants are revamping kids’ menus and loading them with healthier, fresher options. Companies like Walgreens, SuperValu, Walmart, Calhoun’s Grocery are committing to build new stores and to sell fresh food in underserved communities all across this country.
Congress passed historic legislation to provide more nutritious school meals to millions of American children. Our schools are growing gardens all over the place. Cities and towns are opening farmers markets. Congregations are holding summer nutrition programs for their kids. Parents are reading those food labels, and they’re rethinking the meals and the snacks that they serve their kids.
So while we still have a long way to go, we have seen so much good progress. We’ve begun to have an impact on how, and what, our kids are eating every single day. And that is so important. It’s so important.
Really? I’d say we’ve seen promises from food companies but remarkably little action.
Mrs. Obama’s speech fails to mention what I’m guessing is the real reason for the shift: “Move more” is not politically loaded. “Eat less” is.
Everyone loves to promote physical activity. Trying to get the food industry to budge on product formulations and marketing to kids is an uphill battle that confronts intense, highly paid lobbying.
You don’t believe this? Consider recent examples of food industry opposition to anti-obesity efforts:
- Soda companies successfully defeated efforts to impose taxes on soft drinks.
- Food companies successfully defeated efforts by four federal agencies to set voluntary standards for marketing foods to children.
- Food companies successfully lobbied Congress to pass a law forbidding the USDA from setting standards for school meals regarding potatoes, tomato sauce, and whole grains. The result? Pizza tomato sauce now counts as a vegetable serving.
- McDonald’s and Burger King evaded San Francisco’s new rules restricting toys with kids meals by selling the toys separately for ten cents each.
The political cost of fighting the food industry is surely the reason for the change in Mrs. Obama’s rhetoric. Now, she agrees that kids won’t eat vegetables unless forced to.
But in March 2010 Mrs. Obama warned Grocery Manufacturers Association:
We need you…to entirely rethink the products that you’re offering…, the information that you provide about these products, and how you market those products to our children….This isn’t about finding creative ways to market products as healthy.
The food industry understood those as fighting words. It fought back with weapons at its disposal, one of which is to deflect attention from food by focusing on physical activity. It now has White House endorsement of this deflection.
I’m all for promoting physical activity but the refocusing is a loss, not a win, in the fight against childhood obesity.